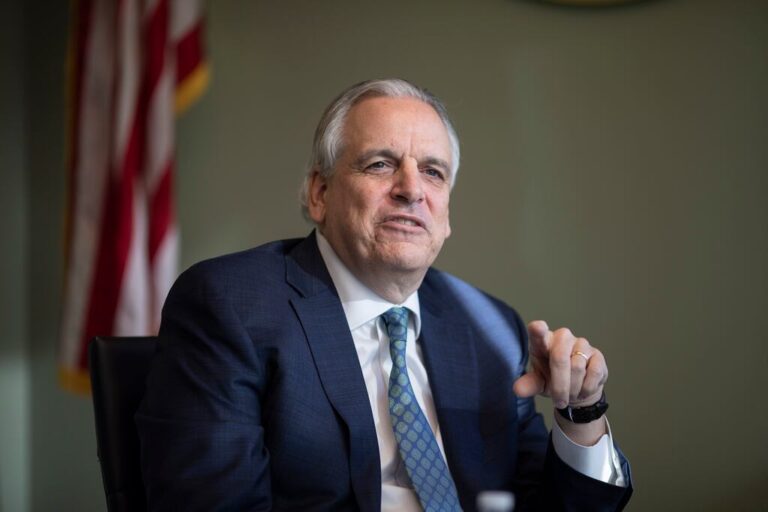
PROVIDENCE — Attorney General Peter Neronha, Brown University Health President and CEO John Fernandez, and Maura Daly Iversen, the dean of the College of Health & Wellness at Johnson & Wales University, painted a bleak picture for the future of hospitals and primary care providers on Wednesday, warning that state leaders need to pour tens of millions of dollars into the system in the near future in order to avoid a collapse.
During a Rhode Map Live event about the state’s health care crisis, Nehrona predicted there could be hospital closures, Rhode Island Hospital and other institutions will have to put off infrastructure improvements, and “you’re not going to have a primary care doctor, or they’re going to keep turning over because they’re going to keep leaving.”
Iversen called it a “very unsettling point in time” for Rhode Island.
“I can’t imagine that the system can persist the way it is situated right now,” she said. “And we need to really look at a team approach with all of the health professionals engaged in this conversation and recruit it to help to address our healthcare needs.”
Fernandez’s appearance drew a small crowd of protesters outside the event, as a contract dispute between the health care system and nurses persists. But during the discussion, Fernandez was the most direct: Without investment, the health care system will be “a simple unmitigated disaster, and it won’t wait two years. It will start in places we don’t like, and just get worse. So we need to fix it.”
A slate of possible actions
Earlier in the day, Neronha unveiled a large slate of actions developed by his office — from legislative proposals to a lawsuit targeting pharmacy benefit managers and a call for a new health policy agency — that he said are urgently needed to correct and stabilize the state’s failing health care system.
“We are in a state today of spectacular failure that is literally occurring before our eyes,” Neronha, a Democrat, said at a press conference at his office in Providence.
Rhode Island is struggling to maintain and expand its number of primary care providers. Drug prices are high. And the survival of Roger Williams Medical Center in Providence and Our Lady of Fatima Hospital in North Providence, following the bankruptcy of Prospect Medical Holdings, is “on the edge of a knife,” Neronha said.
“If they don’t, there will be one reason why not: because we haven’t acted quickly enough,” the attorney general said.
“If we have the courage to do what we’re talking about today, we can drive down costs, enhance revenue, [and] give Rhode Islanders a health care system they deserve,” he added.
On that list is proposed legislation to immediately increase Medicaid reimbursement rates to primary care providers so the rates are 100 percent “on par with rates for Medicare,” officials said. The current Medicaid rate in Rhode Island is 37 percent of Medicare’s rate — lower than it is in neighboring Massachusetts and Connecticut, Neronha said.
“Low Medicaid reimbursement also undercuts our primary care providers by under compensating them for their services, and it makes it harder for Rhode Island to retain PCPs,” said Lee Staley, the health care unit chief for the Attorney General’s Office.
The bill, if approved, “would allow for the state to leverage federal matching funds that are available in the Medicaid program, essentially letting the state’s dollars stretch further,” Staley said.
The initiative is estimated to cost around $50 million, according to Neronha. He said he has spoken with House Speaker K. Joseph Shekarchi about how to drum up the funding, but did not elaborate further.
“We have to stabilize primary care right now,” Neronha said. “Primary care doctors are the air traffic controllers of our health care system. They’re the ones that analyze our problem, send us to the tests we need, send us to the specialist we need.”

Here are other actions Neronha outlined on Wednesday:
A lawsuit against pharmacy benefit managers
Rhode Island has filed a lawsuit in Providence County Superior Court against the country’s largest pharmacy benefit managers — CVS Caremark, Express Scripts, and Optum — and their affiliated group purchasing organizations, Zinc, Ascent Health Services, Emisar Pharma Services.
The lawsuit alleges that PBNs, which act as a third-party between health plans and drug manufacturers, “deceive consumers by branding themselves as a source of cost-savings when, in fact, they profit directly from cost increases,” officials said.
“Often secretive and unknown to consumers, PBMs and GPOs exploit the complex scheme of pricing and payment for prescription drugs, and take a cut of ever-increasing drug prices at every step of the way,” Neronha’s office said. “They may also make decisions about formularies — the lists of drugs that are available to plan enrollees — that unfairly restrict access to safe and effective medications.”
Proposed legislation and regulations
Neronha’s office has proposed legislation that, if passed, would make it unlawful for insurers to require prior authorization “on any procedure, test, treatment, study, or prescription drug ordered by a primary care provider, with exceptions for controlled substances and individual providers with identified cases of fraud, waste, or abuse,” officials said.
Another proposed bill would grant the attorney general the authority to petition the Superior Court to place a hospital into receivership — a process similar to bankruptcy in state court — if it is in “financial distress or is otherwise being operated in a manner that is detrimental to patients,” Neronha’s office said.
Prosecutors are also eyeing regulations to require the attorney general’s office be notified of “certain material corporate transactions involving medical practice groups, including transactions involving private equity firms,” and are looking into how to possibly regulate the use of artificial intelligence in health care, officials said.
Establishing a new state health care agency and Brown University collaboration
The Attorney General’s Office has also collaborated with the Brown University School of Public Health Center for Advancing Health Policy Through Research to “examine potential policy options for state-based health system reform,” officials said.
Additionally, Neronha said his office is proposing the creation of a new state-run health care agency that would work to collect data and make policy recommendations to improve Rhode Island’s health care system.
Officials anticipate a more complete proposal to be ready later this year, before the 2026 legislative session.
“We have come to the conclusion that the way we’re doing health care isn’t strategic — that that element of thinking doesn’t exist in Rhode Island,” he said.
“We can do better,” he added.
Watch Dan McGowan discuss this story on WPRI Channel 12, or in the player above. See more Globe Rhode Island stories that have been featured on Channel 12 here.


Comment count: